Rheumatoid Arthritis
by Stefanie Zinchiak M.Ed.
Medically Reviewed by Dr. Linda Lemay M.D.

Understanding Rheumatoid Arthritis
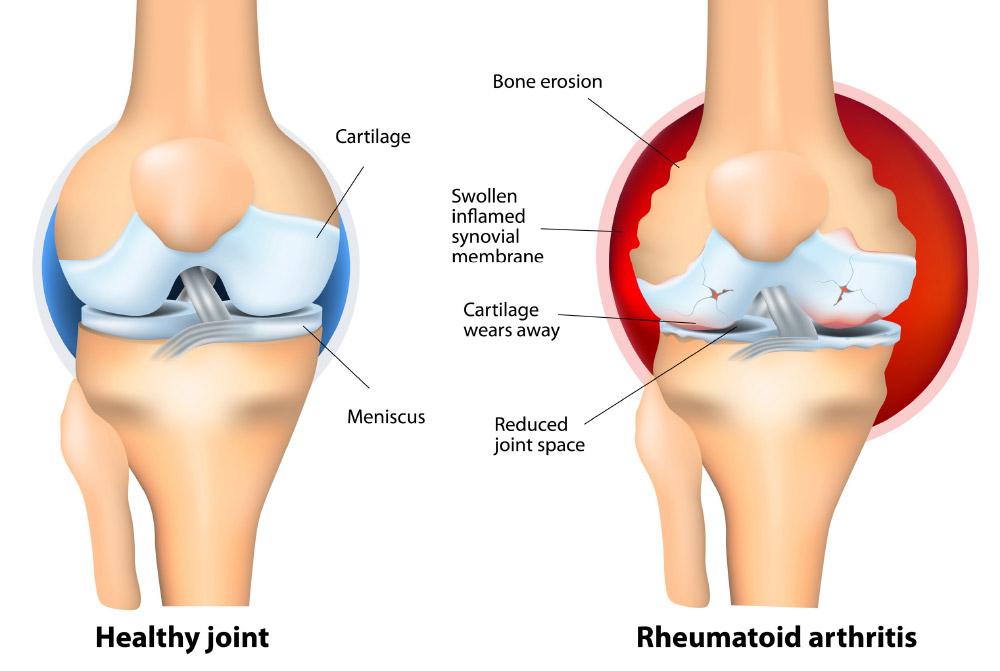
Rheumatoid arthritis (RA) is an autoimmune disease in which the immune system, which typically defends the body from infection, attacks its own joint tissues (synovium). White blood cells travel to the joints causing swelling, puffiness, and pain. As RA progresses, the inflamed synovium wears away the cartilage and erodes the bone within the joint. The surrounding muscles, ligaments, and tendons that support the joint become weak and unable to function normally. These effects lead to pain and joint damage.
The progression of rheumatoid arthritis can range from mild to severe. For many people, there are periods of very mild activity with occasional flare-ups. In others, symptoms of pain, stiffness, swelling, and limited motion can be constant. Rheumatoid arthritis is a chronic, lifetime disease that requires early diagnosis to best manage its effects.
Symptoms
Rheumatoid arthritis can be hard to identify at first because many diseases have similar symptoms in their beginning stages. Common symptoms include:
- Joint soreness, warmth, stiffness, pain, and/or swelling. Some people may also have symptoms in places other than their joints
- Fatigue
- Low fevers
- Loss of appetite
- Dry eyes and/or mouth
- Anemia, or a decrease in the production of red blood cells
- Firm lumps, called rheumatoid nodules, which grow beneath the skin
Causes
This chronic autoimmune disease affects more than 1.3 million Americans, 75 percent of which are women. The main cause of rheumatoid arthritis is unknown, but research suggests that multiple factors may be the culprit.
Scientists have uncovered certain genes that may play a role in a person developing rheumatoid arthritis. Since women are more likely to develop this disease, some scientists also believe that hormones or deficiencies in certain hormones may be a factor. In addition, scientists have speculated about environmental issues that occur to trigger the disease. Currently, there is no single cause that has been identified; however, researchers are continuing to study how these factors affect one another.
Diagnosis
Rheumatoid arthritis can be difficult to diagnose in its early stages because there is no single test for the disease and the symptoms can be similar to many other conditions. As a result, general practitioners or orthopedists use a variety of tools to diagnose the disease:
Medical history: The doctor will ask you to describe how your pain, stiffness, and joint function have changed over time.
Physical examination: Your joints will be examined for redness, swelling, and/ or warmth. Also, the doctor will observe your joint flexibility, muscle strength, reflexes, and ability to carry out daily activities.
Laboratory tests: There is no single test that confirms a rheumatoid arthritis diagnosis; however, most patients who have RA, test positive for Rheumatoid Factor (RF) and/ or Cyclic Citrullinated Peptide (anti-CCP). Other common laboratory tests include a white blood cell count, a blood test for anemia, the erythrocyte sedimentation rate (sed rate), and C-reactive protein.
X-rays: X-rays are used to determine the degree of joint damage and can be used to rule out other causes of joint pain.
Your doctor will make a diagnosis by evaluating the results from the physical exam, medical history, lab tests, and X-rays.
Treatment
The goals of rheumatoid arthritis treatment are to relieve pain, reduce swelling, increase mobility, slow down or stop joint damage, and improve a patient’s daily living. The treatment approaches include a combination of medications, orthopedic surgery, changes in lifestyle, and routine follow-up care.
Medications: Most people who have rheumatoid arthritis take medications for pain relief (analgesics); others, such as corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), are used to reduce inflammation. In addition, disease-modifying antirheumatic drugs (DMARDs), are used to try to slow the progression of the disease.
Surgery: Orthopedic surgical procedures to the joints are done to reduce pain, improve joint function, and improve the patient’s ability to perform daily activities. Some of the more common orthopedic surgeries include:
Joint replacement: Joint replacement is an option for different joints, but the most commonly replaced joints are the hips and knees.
Arthrodesis (fusion): Arthrodesis involves removing the joint and fusing the bones together. Ankles, wrists, fingers, and toes are the most common joints for this surgery.
Tendon reconstruction: This procedure, which is used most frequently on the hands, reconstructs the damaged tendons by attaching a healthy tendon to it.
Synovectomy: In this surgery, the inflamed synovial tissue is removed.
Lifestyle Changes: Rest, exercise, diet, joint care, and stress reduction can help manage symptoms of rheumatoid arthritis. Acupuncture and massage can also help reduce stress and manage symptoms.
Routine Follow-Up Care: Regular visits to your doctor will help to monitor the disease and determine any modifications to treatment. Your doctor will routinely conduct laboratory tests and x-rays to observe the progression of the disease.
Patients who are knowledgeable about RA and monitor their treatment will feel a greater sense of control over the disease. Ultimately, with a combination of treatments and coping skills, those with rheumatoid arthritis can lead a full, active life.
Where to Go
Your primary care physician will order an initial set of tests or screenings, and may prescribe pain-relieving medications or alternative treatments. If additional assessments or treatments are needed, they may give you a referral to a rheumatologist or an orthopedist, depending on your needs. Rheumatologists are internal medicine physicians and focus on autoimmune conditions and non-surgical treatments for arthritis, in which medications and/or physical therapy may prove sufficient. Orthopedists on the other hand, are surgeons who provide surgical treatments for bone and joint diseases like arthritis, osteoarthritis, as well as surgical procedures for injuries.
According to a study reported in The Journal of the American Academy of Orthopaedic Surgeons, structural anatomy differences, hormones, and genetics are factors in optimizing care for male vs. female orthopedic patients. “Women have different orthopedics needs, particularly as they grow older and become more at risk for osteoporosis and fractures. Being treated with the proper level of care impacts one’s health, well-being, and healing, so it is critical for women to know those hospitals that have demonstrated the highest level of quality care for their patients, with a special focus on the needs and preferences of women. said Delia Passi, founder and CEO of the Women’s Choice Award. If you’re in search of an orthopedic surgeon, the Women’s Choice Award America’s Best Hospitals for Orthopedics have met the highest standards for orthopedics across the U.S.
Questions to Ask Your Orthopedist:
Q: How do you know that I have rheumatoid arthritis?
Q: What is my best pain relief option?
Q: Which is the best treatment for me?
Q: Are there any exercises I can do to restore mobility in my joints?
Resources:
America’s Best Hospitals for Orthopedics
Know Where to Go, Know What to Do
The National Library of Medicine
Office on Women’s Health
http://www.womenshealth.gov
This content is for informational purposes only and is not intended to provide medical advice or to treat, diagnose, cure or prevent any disease or condition. Always seek the advice of your healthcare provider.
Sources:
http://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis
http://www.niams.nih.gov/Health_Info/Rheumatic_Disease/default.asp#ra_2
http://www.womenshealth.gov/aging/diseases-conditions/rheumatoid-arthritis.html
Back